Ultrasonography – closing small blood vessels

One of the most common treatments performed in phlebological and aesthetic medi-cine clinics is closing small blood vessels in the lower extremities, so-called telangiec-tasias and reticular vessels. Currently, there are several methods that allow for clos-ing the dilated vessels and obtaining desirable effects, both therapeutic and aesthetic. Unfortunately, despite applying various methods and instruments, the effects of treat-ments are frequently not satisfactory. The factor that largely contributes to decreasing the efficacy of such procedures is complicated anatomy of the venous system and the lack of a method to precisely specify the vessel’s course, its diameter, location in the skin etc. High-frequency ultrasonography is a method enabling accurate determination of the ves-sels’ course as well as the measurement of their basic parameters, such as diameter, depth in the skin and presence or absence of perfusion. Thanks to ultrasound imaging with the use of high-frequency transducers, an adequate treatment method and procedure parameters may be selected, which entails enhancing the efficacy of the procedure itself. Ultrasonography may be also used for monitoring the performed procedures.
Vascular problems in the lower limbs occur very frequently. It is estimated that problems with the venous system of the lower extremities concern approximately 40–50% of the population(1). Unsightly appearance of the legs with multiple telangiectasias and dilated reticular vessels not only constitutes an aesthetic problem, but may also lead to severe health conditions. The procedures consisting in closing small vessels, commonly known as “spider veins,” belong to the most popular treatments performed in phle-bological and aesthetic medicine clinics. The majority of patients, mainly women, do not accept the developing vas-cular changes appearing in the lower extremities and thus, the main reason for treatment is the improvement of their appearance(2).
Vascular changes occurring in the legs are associated with anomalies in the superficial, epifascial venous system. The etiology of these disorders is complex. It is indicated that the most common causes of venous disorders encompass genetic and hormonal factors as well as obesity, lifestyle and pregnancy. These factors lead to the insufficiency of the venous valves and perforators, which makes the blood collect in the vessels as well as causes venous hyperten-sion and results in dilatation of the vessels. We distinguish two main veins in the superficial venous system: great and small saphenous veins as well as multiple perforator veins and small blood vessels(3). In order to systematize the ves-sels that make up the superficial venous system, it appears to be appropriate to use a classification which distinguishes five types of vessels(4). Type I comprises red vessels with the diameter of 1 mm, i.e. telangiectasias. Type IA includes very small red vessels whose diameter is lower than 0.2 mm. These vessels have a “secondary” character (they appear in patients following treatments) and are referred to as matting. Type II encompasses purple vessels with the diameter of 1–2 mm which are raised above the skin sur-face. Type III includes reticular vessels with green and blue coloring and the diameter of 2–4 mm. Type IV comprises varicose veins with 3–8 mm in diameter, unrelated to the vena saphena magna. Finally, type V includes varicose veins of the vena saphena magna and parva with blue or blue-green color and diameter above 8 mm.
The dilated blood vessels in the legs may be eliminated by means of sclerotherapy or various laser treatments. Unfortunately, the efficacy of such procedures is not always satisfactory(2,5), which is a consequence of a com-plex structure of the venous system, constraints of the methods used to close venous vessels and the lack of a method which would enable accurate imaging of the course of the vessels to be treated. In particular, we lack tools enabling imaging of the course of the small blood vessels. In such a situation, it is desirable to search for a method that would allow for accurate imaging of the venous system and thereby, contribute to the efficacy of the performed procedures. High-frequency ultrasound (HFU) has a chance to become a useful tool in imaging of small blood vessels.
For the purposes of this paper, the ultrasound images have been obtained by means of high-frequency equipment, i.e. Episcan with a mechanical transducer of 50 MHz (Longport International, Great Britain, USA), DermaMed with a mechanical transducer of 48 MHz (Dramiński, Poland) and Sonix with an electronic linear array trans-ducer with the frequency of 40 MHz (Ultrasonix, Canada).
Imaging of the superficial venous system
The procedures aiming at eliminating small blood vessels in the lower limbs are not easy and obtaining the outcomes satisfactory for patients may be difficult. In such a situa-tion, an adequate diagnostic process, localizing the prob-lem and selecting an appropriate treatment method are essential.
In the case of patients awaiting the elimination of small blood vessels, it is necessary to perform an exhaustive inter-view and obtain information concerning the incidence of vascular problems in the family, patient’s lifestyle, history of diseases and possible symptoms and ailments which may indicate the presence of chronic venous insufficiency. Another step is Doppler ultrasound (US) examination with the use of broadband linear array transducers with the frequency of 5–12 MHz. Doppler examination plays a vital role in establishing a correct diagnosis and plan-ning further treatment. According to Weiss, Doppler US is as essential as using a stethoscope in a routine physical examination(6). Such an examination enables to assess the patency and sufficiency of the great and small saphenous veins as well as allows for a localization of incompetent veins and perforators. If the examination reveals insuffi-ciency of the great and small saphenous veins, it must be first treated and only then the small vessels may be elimi-nated. Closing of telangiectasias and reticular veins with concomitant insufficiency of the main veins of the super-ficial system is useless because the procedure may occur completely ineffective.
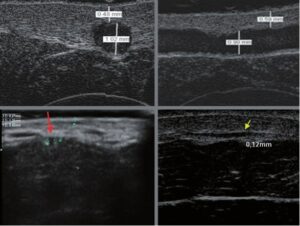
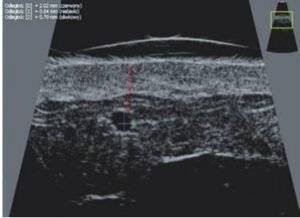
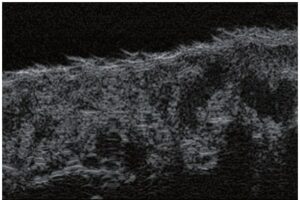
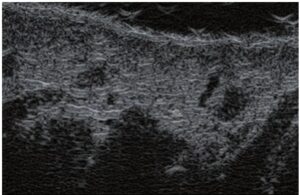
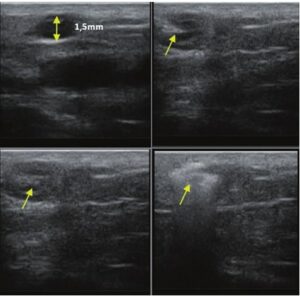
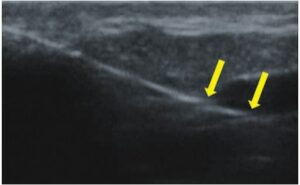
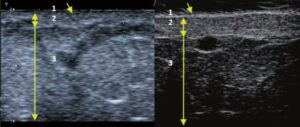
Doppler sonography enables imaging of large vessels and perforators which are usually located in the deeper layers of the subcutaneous tissue (fig. 1). Unfortunately, conven-tional sonography is not capable of imaging smaller ves-sels. In order to visualize smaller vessels located near the surface of the epidermis and in the upper layer of the sub-cutaneous tissue, HFU is used (fig. 1). Thanks to the usage of transducers with frequencies higher than 20 MHz, a high resolution ultrasound image is obtained in which we may differentiate between structures that are smaller than 0.1 mm. However, the higher the resolution, the shal-lower the penetration of the ultrasound beam into the skin layers. Therefore, depending on the transducer and appa-ratus, it is possible to penetrate the skin to the depth of max. 20–30 mm. Such a penetration, together with high image resolution, enables the assessment of even very small blood vessels (fig. 2). During the examination with the use of high-frequency transducers, one may precisely assess the course and location of the small vessels in the skin. This is particularly relevant for the selection of the vessel closing method and planning the procedure since in practice, the surface of the skin very often shows solely a small number of vessels or a slight fragment of a ves-sel – only after US examination may we determine their actual number and course. For an effective closing of the vessel, it is necessary to do it on its entire length. It must not be limited to the fragment seen “with the naked eye” on the surface of the skin since closing of the fragment will cause its swift recanalization(7). Frequently, the ves-sel visible on the surface of the skin changes its course, becomes more tortuous and travels to the deeper layers of the skin(8). Therefore, the vein’s course and the per-forators should be well-known and determined prior to the procedure. HFU also enables imaging of the perfora-tors between small vessels. Furthermore, apart from the assessment of the course and anatomy, ultrasound image, thanks to the ultrasound software, also enables to deter-mine the basic parameters such as the vessel’s diameter, thickness of its wall, depth in the skin as well as presence or absence of perfusion inside the vessel(6) (fig. 3). Thanks to the multi-element electronic transducer with the fre-quency of 40 MHz introduced to the market by Ultrasonix, it is also possible to visualize perfusion in the vessels in the color Doppler mode (fig. 4).
Treatments eliminating small blood vessels
Currently, small blood vessels are closed by means of microsclerotherapy, surface laser treatments as well as micro-endovascular procedures(7).
Laser therapy
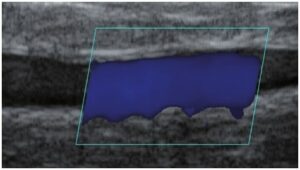
Laser treatments consisting in a transcutaneous clos-ing of the vessels are becoming more and more popular. The essence of these treatments lies in sending a light beam onto the vessel, which is absorbed by hemoglo-bin contained in erythrocytes and transformed into heat energy. This leads to heating of the vessel wall and its coagulation. Whereas in slight telangiectasias, the effect is obtained immediately, in reticular veins, the closing occurs several weeks following the procedure(9). The efficacy of the therapy depends on adequate selec-tion of the treatment parameters. Determining the loca-tion of the vessels in the skin layers and their diameters are of great significance. These two parameters may be accurately specified in HFU. Based on US findings, the type of laser is selected, which entails the selection of wave length, pulse width, diameter of the spotsize and pulse energy(7). In laser therapy, HFU is also useful as a method for monitoring the correctness of the treatment and its effectiveness. During the procedure, US may help to ensure that the laser energy reaches the vessel – its diameter should decrease at once (fig. 5). When such an effect is not detected, the treatment parameters should be verified. Additionally, it should be checked whether the laser head is adequately applied to the skin. HFU is also used for assessing the effectiveness of performed proce-dures. The useful parameters in such an assessment are: presence or lack of perfusion in the vessel, presence or absence of a thrombus in the vessel’s lumen, diameter of the vessel and thickness of its wall.
Sclerotherapy
Sclerotherapy is a technique of closing vessels as a result of injecting them with a chemical sclerosant. At present, it is commonly applied and is characterized by, above all, low costs and the fact that it is relatively easy to perform. Sclerotherapy is primarily indicated for closing reticular veins that are greater than 3 mm but may also be applied if the vessels are smaller(10). In the case of vessels smaller than 3 mm, it is more difficult to insert a needle to their lumina, which increases the risk of complications(7). In such a situation, HFU occurs to be helpful. It allows for accurate visualization of the vessel’s course and, sub-sequently, facilitates the performance of the procedure with US-guidance (fig. 6). Thus, thanks to ultrasonogra-phy, the risk of administering the sclerosant beyond the vessel’s lumen, which entails necrosis, has been elimi-nated. High-frequency ultrasound imaging may also be used to monitor the efficacy of the procedure.
Micro-endovascular procedure
Micro-endovascular procedure is an endovenous technique which was primarily used for the treatment of insufficiency of large veins in the superficial system and which has been adapted for smaller veins. It is currently used in closing reticular veins and telangiectasias. The procedure con-sists in inserting a sterile laser optical fiber and inducing coagulation of the vessels as a result of laser energy(7,11). It requires high-frequency ultrasound-guidance. Owing to ultrasound imaging, it is possible to assess the vessel’s course and anatomy, accurate insertion of the optical fiber to the vessels (fig. 7), coagulation of the vessel and efficacy of the procedure.
Conclusion
This paper has presented the subject-matter related to the application of HFU in imaging and closing of small venous vessels, i.e. telangiectasias and reticular veins. The introduction of high-frequency transducers of above 20 MHz made it possible to visualize the vessels located in the dermis and subcutaneous tissue, which is not fea-sible with the use of conventional probes or other meth-ods. Sonography as a method of small vessel imaging ful-fills the expectations of surgeons and phlebologists who, until now, have been deprived of the possibility to evalu-ate small blood vessels. Diaphanoscopes (transillumina-tors) had limitations since they only enabled to assess the course of shallow vessels(12) without the possibility to specify their exact location or diameter. However, the pos-sibility to assess the course of vessels, measure their diam-eters and specify their location in the skin contributes to the selection of a therapeutic method. Thereby, these fac-tors enhance the efficacy of the selected procedure and reduce the risk of complications. In the case of laser treat-ments, ultrasound images facilitate the selection the laser for a procedure and enable to determine the treatment parameters(7). Sonography is also useful as a method of monitoring the procedures that aim at elimination of the vessels. Without ultrasound imaging, the performance of certain procedures would not be feasible, for instance, micro-endovascular procedures without ultrasound guid-ance or microsclerotherapy without ultrasound imaging of the small vessels. The latter procedure performed with-out ultrasound guidance is burdened with a large risk of complications in the form of necrosis caused by adminis-tering the sclerosant beyond the vessel’s lumen.
As has been shown above, high-frequency ultrasonogra-phy is a useful method in imaging of small blood vessels. Due to a relative low cost of the examination or of high-frequency equipment as compared with other methods, such as computed tomography or magnetic resonance imaging, as well as because of its non-invasive char-acter, mobility, relatively easy scanning technique and possibility to repeat examinations safely for the patients, HFU has a chance to become a more widely used routine examination.
Conflict of interest
Authors do not report any financial or personal links with other per-sons or organizations, which might affect negatively the content of this publication and/or claim authorship rights to this publication.
References
- Munavalli GS, Weiss RA: Objawy chorób żył. In: Alam M, Nguyen TH (eds.): Leczenie chorób żył kończyn dolnych. Elsevier Urban & Partner, Wrocław 2009: 11–25.
- Rohrer TE, Geronemus RG, Berlin AL: Zmiany naczyniowe. In: Gold-berg DJ (ed.): Lasery i światło. Vol. 1, Elsevier Urban & Partner, Wro-cław 2009: 1–16.
- Somjen GM: Anatomy of the superficial venous system. Dermatol Surg 1995; 21: 35–45.
- Weiss AR, Weiss MA: Painful telangiectasias: diagnosis and treatment. In: Bergan JJ, Goldman MP (eds.): Varicose Veins and Telangiectasias: Diagnosis and Treatment. Quality Medical Publishing, Inc., St. Louis 1993: 389–406.
- McCoppin HH, Hovenic WW, Wheeland RG: Laser treatment of super-ficial leg veins: a review. Dermatol Surg 2011; 37: 729–741.
- Weiss RA: Badanie pacjenta: wywiad i badanie przedmiotowe. In: Alam M, Nguyen TH (eds.): Leczenie chorób żył kończyn dolnych. Else-vier Urban & Partner, Wrocław 2009: 27–41.
- Mlosek R: Przydatność badań ultrasonograficznych w zamykaniu drob-nych naczyń krwionośnych. In: Mlosek R: Obrazowanie skóry i tkanki podskórnej za pomocą ultrasonografii klasycznej oraz ultrasonografii wysokich częstotliwości i jego przydatność w kosmetologii i medycynie estetycznej. Oficyna Wydawnicza Warszawskiego Uniwersytetu Medycz-nego, Warszawa 2012: 133–154.
- Hsu J, Bhatia A, Weiss R: Naczynia żylne kończyn dolnych. In: Gold-berg DJ (ed.): Lasery i światło. Vol. 1, Elsevier Urban & Partner, Wro-cław 2009.
- Bogle M, Sadick N: Zabiegi laserowe. In: Alam M, Nguyen TH (eds.): Leczenie chorób żył kończyn dolnych. Elsevier Urban & Partner, Wro-cław 2006: 101–118.
- Duffy DM: Skleroterapia. In: Alam M, Nguyen TH (eds.): Leczenie chorób żył kończyn dolnych. Elsevier Urban & Partner, Wrocław 2006: 67–99.
- Sznelewski P, Rybak W: Światłoterapia wysokoenergetyczna we fle- In: Rybak Z (ed.): Flebologia – co nowego? Cornetis, Wrocław 2012: 191–197.
- Pszenny C: Problemy naczyniowe kończyn dolnych. In: Mamcarz B, Prandecka D (eds.) Medycyna estetyczna w praktyce. Vol. 1, Medical Education Sp. z o.o., Warszawa 2010: 133–142.
Robert Krzysztof Mlosek1, Sylwia Malinowska2
- Department of Medical Imaging, Second Faculty of Medicine, Medical University of Warsaw, Warsaw, Poland
- Life-Beauty private partnership, Grodzisk Mazowiecki, Poland Correspondence: Department of Medical Imaging, Second Faculty of Medicine, Medical University of Warsaw, Kondratowicza 8, 03-242 Warsaw, Poland,
e–mail: zdo@usgptu.waw.pl, tel. +48 22 326 58 10